Scientists assumed for many decades that misguidance was the crux of the problem when the immune system’s attack cells went awry and assaulted the body’s own tissues, causing autoimmune conditions like lupus, diabetes, arthritis, and allergies.
But a theory now gaining widespread favor suggests a more complicated picture with new possibilities for treatments that ease or prevent autoimmune disorders.
“We used to think of mature immune cells like T cells and B cells as metabolically inactive when waiting for infections or other signals that trigger an attack,” says Stanford Peng, M.D., Ph.D., assistant professor of internal medicine and of pathology and immunology at Washington University School of Medicine in St. Louis. “We’re now thinking these resting cells actually are very active but are kept in a quiescent state by genes actively working to shut down activating proteins.”
Peng, who earlier this year discovered the first of these immune system “leashes” in T cells, now has given the theory another key boost by identifying the first leash in a B cell: a protein called microphthalmia-associated transcription factor (MITF). He reported the discovery in the Journal of Experimental Medicine.
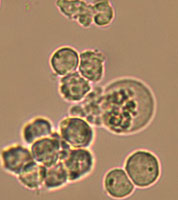
Peng’s research group compared levels of messenger RNA for various genes in the cells of normal mice to mice with lupus-like conditions. Messenger RNA acts like an order slip for the production of a copy of a gene’s protein, so scientists believe levels of messenger RNA for a particular gene are likely to be representative of that gene’s level of activity in a cell.
They found that MITF was much less active in the B cells of mice with lupus-like conditions than in normal mice. When they suppressed MITF activity in normal mice, B cells turned themselves on and began making antibodies, clumps of proteins normally designed to attack invaders. But the new antibodies in the mice were autoantibodies — antibodies targeted to the body’s own tissues that are a characteristic symptom of lupus.
“This is the first transcription factor we’ve found that has to be active in the resting B cell to keep it that way,” says Peng, who is also a physician at Barnes-Jewish Hospital.
MITF appears to exert its leash-like effect by restraining interferon regulatory factor 4 (IRF4), a protein previously linked to the activation of B cells. But it appears to have that effect through its influence on several other genes that in turn act to keep IRF4 in check.
Peng and colleagues are working to further understand how MITF works, and they have also begun looking for signs of abnormal MITF activity in human patients.
“We’ve been focusing our efforts to develop new treatments for autoimmune disease on pathological targets — genes that are overused or used inappropriately, leading to immune system attacks on self,” Peng says. “Another concept we should keep in mind is that the loss of one of these regulatory genes that keep the immune cells in check also may contribute to autoimmune disease.”
Ling L, Gerth AJ, Peng SL. Active inhibition of plasma cell development in resting B cells by microphthalmia-associated transcription factor. Journal of Experimental Medicine, pp. 115-122, July 2004.
Funding from the National Institutes of Health, the Lupus Research Institute, the Arthritis Foundation, and Washington University School of Medicine.
Washington University School of Medicine’s full-time and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked second in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.