A procedure known as lung-volume reduction surgery (LVRS) appears to improve overall health and quality of life for individuals with end-stage emphysema, and these effects last as long as five years in more than half of this population, according to researchers at Washington University School of Medicine in St. Louis.
“Nearly half of all patients with severe emphysema will die within three to five years of diagnosis, and in these years, quality of life will be compromised by shortness of breath and the inability to do everyday tasks,” says Roger D. Yusen, M.D., assistant professor of medicine. “We now have studies demonstrating that LVRS improves lung function and quality of life for a large proportion of patients over a significant period of time.”
The procedure was developed at the School of Medicine in 1993 by Joel D. Cooper, M.D., the Evarts A. Graham Professor of Surgery and head of the Division of Cardiothoracic Surgery. Cooper and Yusen published the latest findings in the March issue of the Journal of Thoracic and Cardiovascular Surgery and in the April issue of the journal Chest.
“This surgery is overwhelmingly successful in some patients with severe emphysema, and these latest findings confirm and underscore its potential for treating this critically ill population,” Cooper says. “These publications represent a major, interdisciplinary team effort, which depended on expertise from a variety of areas, including pulmonary medicine, anesthesiology and nurse coordination.”
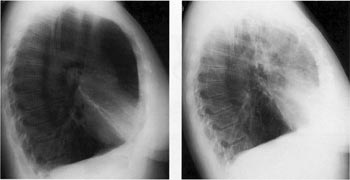
Emphysema is characterized by destruction and overinflation of the lungs. As the lungs become progressively bloated, they fill the chest cavity and thorax, making it difficult to expand and contract during normal breathing. The disease progresses relentlessly and is responsible for close to 17,000 deaths each year in the United States, according to the National Center for Health Statistics.
In patients whose emphysema is particularly bad in localized areas of the lung, LVRS provides an alternative to lung transplantation, which until recently was the only option for patients with end-stage lung disease that cannot be controlled with medical therapy. By removing these most diseased portions of lung, the procedure allows the remaining lung to function better.
Although LVRS is not a cure for emphysema, studies suggest that the surgery increases breathing capacity by more than 50 percent. Such improvements allow otherwise debilitated individuals to resume many normal, daily activities, including moderate exercise. The current studies are the first to examine the long-term endurance of these effects.
The research team maintained a detailed database of lung function and quality-of-life assessments for all patients who underwent LVRS at Washington University’s clinical affiliate, Barnes-Jewish Hospital, between January 1993 and June 2000. Follow-up evaluations were performed six months and one year after surgery and again each year afterward. Patients were followed for an average of 4.8 years.
All participants first were enrolled in a rehabilitation program for about three months prior to surgery and were given medical and dietary programs to make sure they were as healthy as possible for the operation. They also remained on fitness and medical regimens after surgery.
At the conclusion of the study, almost 70 percent of the patients were still alive, and only seven percent had received a lung transplant since undergoing LVRS. Without surgery, it is estimated that half of the patients would have died within three years and most, if not all, would have deteriorated significantly.
Overall, those that survived still had measurable improvements in lung function. For example, patients were tested to see how much air they could blow out in one second, a measurement known as forced expiratory volume 1 (FEV1). Six months after surgery, 95 percent of patients had improved on this test by an average of 54 percent. After five years, 53 percent of patients still had higher levels of FEV1 than before surgery, though the improvement averaged only 7 percent.
Those who survived also had less shortness of breath, with over 70 percent reporting that they were the same or better than before surgery even after five years. Quality-of-life assessments also were positive: Almost 80 percent of patients still reported better quality-of-life scores five years after surgery than before surgery. As a result of these combined improvements, more than 85 percent of these patients were satisfied with the overall surgery after five years.
“This procedure is not a cure for emphysema,” Cooper emphasizes. “No matter how successful the operation, emphysema continues to degrade the lungs and progressively impairs breathing. However, our results confirm that LVRS can in fact extend patients’ lives and allow them to continue participating in normal activities of ‘daily living’.”
Determining selection criteria is one of the most controversial issues in measuring the effectiveness of LVRS. Cooper’s team found that individuals who required surgery to the lower portion of the lungs also benefited from the procedure, but their lung function degraded faster than in individuals with damage to the upper portion of the lungs. Other identified risk factors for worse outcome included advanced age, male gender and very low FEV1.
“We strongly believe that patient selection is one of the keys to success for this procedure,” Cooper says. “With rigorous preoperative preparation and stringent participation criteria, lung-volume reduction surgery appears to improve life expectancy and quality of life for patients who otherwise have very poor prognoses.”
Ciccone AM, Meyers BF, Guthrie TJ, Davis GE, Yusen RD, Lefrak SS, Patterson GA, Cooper JD. Long-term outcome of bilateral lung volume reduction in 250 consecutive emphysema patients. Journal of Thoracic and Cardiovascular Surgery, vol. 125, pp. 513-525, March 2003.
Yusen RD, Lefrak SS, Gierada DS, Davis GE, Meyers BF, Patterson GA, Cooper JD. A prospective evaluation of lung volume reduction surgery in 200 consecutive patients. Chest, vol. 123, pp. 1026-1037, April 2003.